A straightforward addition to routine abdominal operations could prevent thousands of Australian women from developing ovarian cancer, according to leading medical experts pushing for widespread adoption of the procedure.
The Fallopian Tube Connection
Groundbreaking research has revealed that approximately 65 per cent of ovarian cancers actually originate in the fallopian tubes before spreading to the ovaries. This discovery has transformed medical understanding of how this deadly cancer develops.
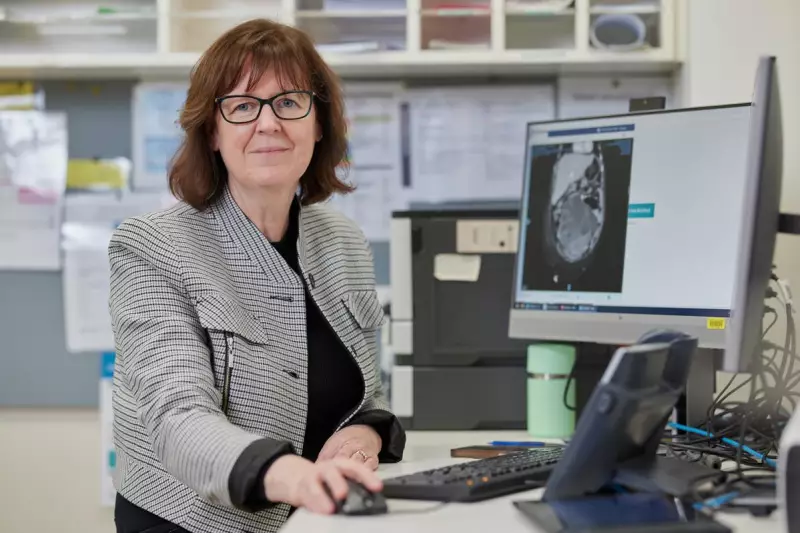
Associate Professor Orla McNally, Director of Gynaecological Oncology at the Royal Women's Hospital in Melbourne, is spearheading efforts to make opportunistic salpingectomy - the removal of fallopian tubes - a standard offering during other abdominal surgeries.
"From published research, it's been established that 65 per cent of ovarian cancers probably start in the fallopian tubes and, in particular, the type of cancer that is usually aggressive and often diagnosed at a later stage," Professor McNally explained.
A Missed Opportunity
A recent United States study published in August 2025 uncovered a concerning statistic: among 1,877 women who developed high-grade serous carcinoma (HGSC), a quarter had previously undergone abdominal surgery where their fallopian tubes could have been removed but weren't.
Dr Amy Wilson, senior research advisor at the Ovarian Cancer Research Foundation, described opportunistic salpingectomy as "the most effective prevention strategy we have at the moment."
"The decrease in risk really varies per study, but it's up to 70 per cent, which is incredible," Dr Wilson emphasised.
Canadian modelling suggests that routinely offering this procedure during abdominal surgery could prevent one in five ovarian cancer cases.
Implementation Challenges in Australia
Despite the compelling evidence, several barriers prevent widespread adoption in Australia. Dr Wilson identified that limited capacity and training among non-gynaecological surgeons, combined with insufficient awareness among both medical professionals and the public, are primary obstacles.
"You need to train surgeons to take out the fallopian tubes safely whilst preserving the ovaries," Dr Wilson noted. "So while they're not trained, it really is something for women to talk about with their doctor and say 'hey, is this a possibility?'"
The procedure itself adds only about 15 minutes to operations women are already undergoing, such as hernia repairs or gallbladder surgery, according to Professor McNally.
"It is considered a low-risk procedure for someone who is having another procedure by a surgeon skilled in those other operations that they're going to be doing," she assured.
Economic and Health Impacts
The potential benefits extend beyond health outcomes to significant economic savings. The financial cost of ovarian cancer treatment in Australia amounts to approximately $66,000 annually per patient, with the total economic burden - including lost productivity and premature death - exceeding $3 billion each year.
"So even if you're reducing a fifth of ovarian cancer cases, which doesn't sound like a lot, that's a huge win for our economy," Dr Wilson added.
Ovarian cancer remains particularly deadly in Australia, with around 1,815 diagnoses and approximately 1,000 deaths annually. The absence of an early detection test and vague symptoms mean 70 per cent of cases are diagnosed only after the cancer has spread to other body parts.
The average five-year survival rate for ovarian cancer stands at just 49 per cent, starkly contrasting with 92 per cent for breast cancer and 74 per cent for cervical cancer.
Current Guidelines and Future Directions
The Royal Australian and New Zealand College of Obstetricians and Gynaecologists already recommends offering fallopian tube removal to women at average ovarian cancer risk during hysterectomy or sterilisation procedures.
Professor McNally advocates extending this practice to other types of abdominal or pelvic surgery for women who have completed their families, typically from age 45. She emphasised that the procedure is irreversible regarding fertility but does not induce menopause since the ovaries remain intact.
This preventive approach has already been implemented in several countries including Canada, Germany, Austria and Sweden for women not planning future pregnancies.
Bridget Bradhurst, acting chief of support and advocacy at Ovarian Cancer Australia, stressed the importance of exploring risk reduction methods given the absence of early detection tests.
"It is great to know that more people are exploring this option with their surgical team, and we look forward to continuing to work with the clinical community to help put recommendations into practice, so women have more options to manage their ovarian cancer risk," she said.
A Western Australian Health spokeswoman confirmed that no systemwide policy or approach to opportunistic salpingectomy currently exists, with procedures only provided when clinically necessary.
The most commonly reported ovarian cancer symptoms include increased abdominal size or persistent bloating, abdominal or pelvic pain, feeling full after eating small amounts, and frequent or urgent need to urinate.